The Brain’s Remarkable Adaptability
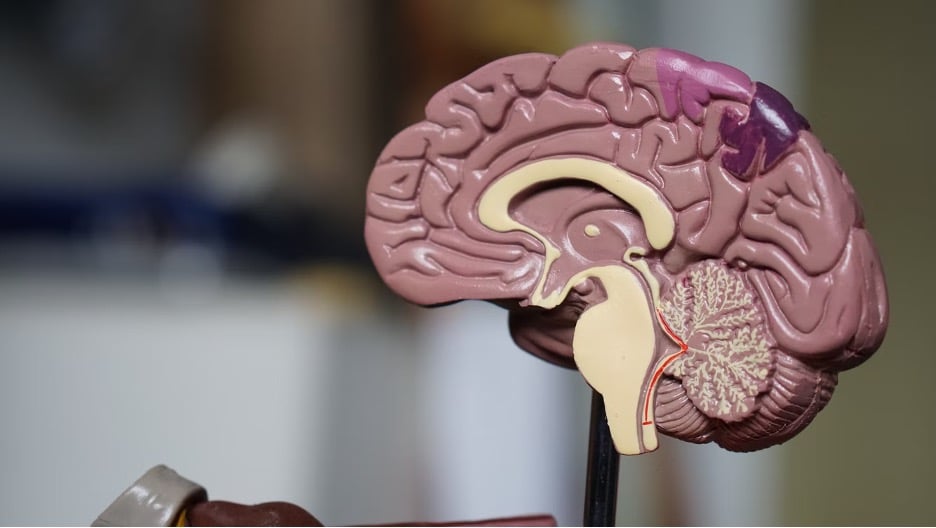
The human brain is a remarkable organ, capable of remarkable adaptability and change throughout one’s lifetime. This property, known as neuroplasticity, allows the brain to reorganize and rewire its neural pathways in response to changes in behavior, environment, and even injury. Harnessing the power of neuroplasticity has become a vital area of research in the field of mental health, as it offers new avenues for treating a wide range of disorders, from depression to chronic pain.
One of the innovative techniques being explored to leverage neuroplasticity is transcranial magnetic stimulation (TMS). TMS is a non-invasive procedure that uses magnetic fields to stimulate specific areas of the brain, triggering changes in neural activity and promoting the formation of new connections. By targeting areas of the brain associated with various mental health conditions, TMS has shown promise in alleviating symptoms and improving overall well-being.
Understanding the Mechanism of TMS
The underlying mechanism of TMS is rooted in the brain’s ability to adapt and change. When a magnetic field is applied to the brain, it produces an electric current that can either excite or inhibit the activity of neurons in the targeted region. This fluctuation in neural activity can set off a cascade of events, leading to the strengthening or weakening of synaptic connections between neurons.
Over successive TMS sessions, these changes in neural connectivity can become more established, effectively “rewiring” the brain’s circuitry. This process of neuroplasticity is crucial in the treatment of mental health conditions, as it allows the brain to adapt and overcome the dysfunctional patterns that contribute to symptoms.
Clinical Applications of TMS
The versatility of TMS has led to its application in the treatment of a growing number of mental health conditions. Perhaps the most well-studied and widely-accepted use of TMS is in the treatment of major depressive disorder. By targeting the dorsolateral prefrontal cortex, an area of the brain associated with mood regulation, TMS has been shown to alleviate symptoms of depression in a significant number of patients.
Beyond depression, TMS is also being explored as a treatment for other conditions, such as anxiety disorders, obsessive-compulsive disorder, and chronic pain. In the case of TMS for anxiety, for example, it may be used to target the amygdala, a brain region known to play a key role in the processing of emotional responses. By modulating the activity of the amygdala, TMS may help to reduce the intensity of anxious thoughts and feelings.
The Future of TMS and Neuroplasticity
As research into the applications of TMS and neuroplasticity continues to evolve, the potential for this approach to transform mental health treatment is becoming increasingly clear. Ongoing studies are exploring the use of TMS in combination with other therapies, such as cognitive-behavioral therapy, to enhance the overall effectiveness of treatment.
Moreover, advances in neuroimaging and computational neuroscience are allowing researchers to better understand the complex neural networks underlying various mental health conditions. This, in turn, is enabling the development of more targeted and personalized TMS protocols, tailored to the unique needs of each individual patient.
Overcoming Limitations Of TMS
While the potential of TMS and neuroplasticity is undeniable, the technology is not without its limitations. One of the key challenges is the precise targeting of the desired brain regions, as the magnetic fields generated by TMS can have a relatively broad reach, potentially affecting areas beyond the intended target. Researchers are exploring ways to enhance the spatial resolution of TMS, such as using novel coil designs and advanced imaging techniques, to improve the precision and efficacy of the treatment.
Another area of ongoing research is the optimization of TMS protocols. The frequency, intensity, and duration of TMS sessions can all impact the resulting neuroplastic changes, and finding the ideal parameters for each individual patient is crucial. Personalized approaches, informed by neuroimaging and computational models, are being developed to tailor TMS treatments to the unique needs and brain characteristics of each patient.
Expanding the Horizons of TMS
As the understanding of TMS and neuroplasticity deepens, researchers are also exploring the potential of this technology to address a wider range of mental health and neurological conditions. Emerging applications include the use of TMS in the treatment of traumatic brain injury, stroke rehabilitation, and neurodegenerative diseases, such as Parkinson’s and Alzheimer’s.
Moreover, the integration of TMS with other technologies, such as virtual reality and brain-computer interfaces, is opening up new avenues for neuromodulation and cognitive enhancement. These hybrid approaches hold the promise of creating more immersive and personalized therapeutic experiences, further empowering individuals in their journey towards better mental health and well-being.
Conclusion: A Transformative Future for Mental Health
The intersection of TMS and neuroplasticity represents a pivotal moment in the field of mental health. By harnessing the brain’s remarkable ability to adapt and change, clinicians and researchers are laying the groundwork for a future where mental health disorders are not just managed, but actively transformed. As the technology continues to evolve and the understanding of the underlying mechanisms deepens, we can look forward to a time when mental health care is more effective, personalized, and truly transformative, empowering individuals to thrive and reach their full potential.
Interesting Related Article: “Meditation: One Thing to Start Doing Today to Keep Your Mind Healthy“