Excess weight cost the US economy $1.7 billion in 2016, says a Milken Institute study. The cost included a $1.24 trillion loss in productivity. Excess weight refers to humans who are either obese or overweight.
According to WHO, an overweight person has a Body Mass Index (BMI) of 25 to 29.9. Obese people have a BMI of 30+. BMI is the ratio of weight (in kilograms) to height (in meters squared) – kg/m2. WHO stands for the World Health Organization.
The amount, $1.7 trillion, represents 9.3% of US GDP. GDP stands for gross domestic product. Milken Institute researchers carried out a study on the role of obesity and overweight in the cost and prevalence of chronic diseases.
According to the study – ‘ America’s Obesity Crisis: The Health and Economic Impact of Excess Weight’ – $1.7 trillion includes:
- Lost productivity: $1.2 trillion.
- Direct health-care costs: $480.7 billion.
The study drew on research that showed how obesity and overweight raised the risk of diseases such as osteoarthritis and heart disease. Excess weight also increases the risk of developing breast cancer.
The research team estimated the cost of lost productivity and medical treatment for each disease.
Excess weight – lost productivity and treatment costs
The treatment cost, for example, for all type 2 diabetes patients was $121 billion while indirect costs were $215 billion. Diabetes Type 2 is one of the most prevalent chronic diseases among overweight/obese people in America.
Treatment costs and productivity costs per person with diabetes type 2 came to $7,109 and $12,633 respectively.
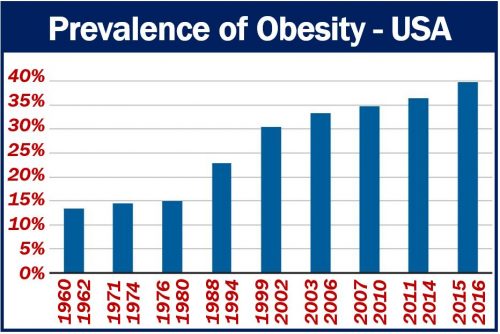
steadily since the 1960s – from 13.4 percent in 1962 to 39.8 percent in 2016.” (Image: adapted from the Report. Data Source: CDC)
The Report focuses on the role excess weight plays in the prevalence of 23 chronic diseases. It also focuses on the resulting economic consequences.
Obesity is linked to, for example, 75% of osteoarthritis and 73% of kidney disease cases. It is also linked to 64% of Type 2 diabetes cases.
Dr. Hugh Waters says the study suggests that weight-control programs could help reduce both the economic and health burdens of chronic diseases. Dr. Waters is Director of Health Economics Research at the Milken Institute.
Dr. Waters said:
“Despite the billions of dollars spent each year on public health programs and consumer weight-loss products, the situation isn’t improving. A new approach is needed.”
Consequences of excess weight
The impact of excess weight on chronic disease is not limited just to the stress that extra weight places on the body.
Research suggests, for example, that fat cells secrete hormones that increase insulin resistance and trigger inflammation.
These reactions can subsequently contribute to a higher risk of developing type 2 diabetes. They can also increase the risk of developing some cancers and cardiovascular diseases.
Thirty-three percent of Americans were overweight but not obese, and almost 40% were obese in 2016, says the CDC. CDC stands for the Centers for Disease Control and Prevention.
The percentages have risen steadily since 1962. In 1962, just 32% of Americans were overweight, and 13% were obese.
Direct medical costs vs. indirect costs
Direct medical costs include:
- Payments that patients and their families make to treat the disease in question.
- Employers’ payments.
- Payments from insurance companies.
Indirect costs include the economic impact of:
- Absence from work.
- Lost income (wages).
- Lost productivity of patients as well as caregivers.

