Doctors prescribe a wide range of lupus medications. However, although drugs help ease or control the symptoms, none of them can cure the disease. In other words, lupus is incurable.
Nobody knows for certain what causes lupus. Experts believe it is due to a combination of environmental, hormonal, and genetic factors.
The earlier treatment can begin, the more effective lupus medications are.
Lupus has several different possible signs and symptoms. The disease can affect many parts of the body. That is why we call it a ‘systemic‘ disease. ‘Systemic’ refers to the ‘whole system,’ which in this case means the human body.
The global pharmaceutical market for the disease is huge, partly because doctors use so many different lupus medications. It is also a huge market because lupus is a chronic disease. Chronic means long-term. When you develop lupus, you have it for life.
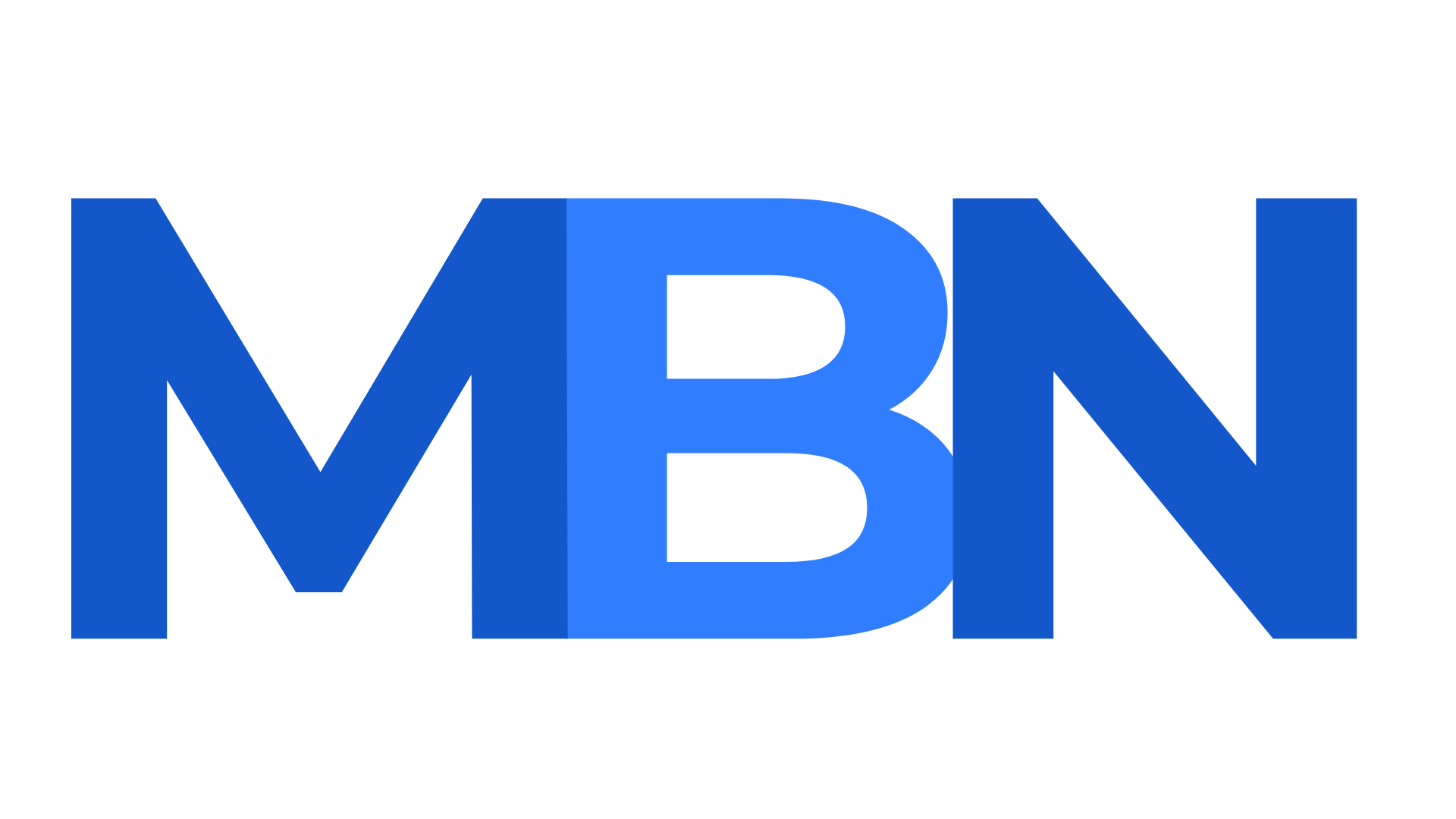
Types of lupus medications
Below is a list of the most common lupus medications, plus information about them.
Anti-inflammatories – pain relief
Anti-inflammatories are the most common lupus medications. Not only do they help reduce inflammation, but they also provide pain relief.
Patients also take anti-inflammatories for arthritis, pleurisy, and fever. Pleurisy is inflammation of the pleura, i.e., the linings around the lungs.
A significant proportion of lupus patients report that they only take an anti-inflammatory to control the disease – they take nothing else.
Aspirin
Patients use aspirin or acetylsalicylic acid to treat inflammation, fever, and pain. It is also an anticoagulant, i.e., it thins the blood.
If you have salicylate intolerance or are allergic to naproxen or ibuprofen, you should not take aspirin. People with NSAID-precipitated bronchospasm or asthma need to be cautious.
Aspirin can also raise the risk of gastrointestinal bleeding.
Aspirin is an NSAID. NSAID stands for non-steroidal anti-inflammatory drug. It is a class of analgesic medication that relieves pain and reduces inflammation and fever. Apart from aspirin, ibuprofen, celecoxib, and naproxen are also NSAIDs.
Acetaminophen (paracetamol)
In the English-speaking countries, lay people have different words for acetaminophen. The most common term in the United States is Tylenol, while Britons and Irish people say ‘paracetamol.’
Acetaminophen helps reduce pain but not inflammation. It cannot control or reduce lupus disease activity either.
A very rare side-effect is acute liver failure. Liver failure tends to occur only among patients who overdosed on acetaminophen. Another extremely rare side effect is toxic epidermal necrolysis.
Ibuprofen
Patients take ibuprofen for pain relief or inflammation. They also take it to bring down a fever.
Ibuprofen can cause heartburn as well as a skin rash. However, compared to other NSAIDs, it has fewer side effects.
Naproxen
People take naproxen to relieve stiffness, inflammation, fever, and pain. It is an NSAID of the propionic acid class. Ibuprofen is also of the propionic acid class.
Side effects include headache, dizziness, bruising, heartburn, and possibly a skin rash.
According to anecdotal evidence from Lupus chat rooms, people tend to either love or hate this medication.
The following quote comes from Lupus UK:
“I would totally recommend naproxen tablets. I recently got put on them last year in December and I’ve noticed a massive difference to my joint pain; I’m not as stiff, sore or swollen as what I used to be and I feel much more free.”
“I had been taking nearly eight painkillers a day since I was a teenager and now I’m 27 and wish I had been put on naproxen earlier.”
This patient, on the other hand, does not seem to like the medication (quote is also from Lupus UK):
“I have felt ‘weird’ and kind of spaced out after each time! I don’t like taking anything that makes me feel different.”
Corticosteroids
Corticosteroids or steroids are anti-inflammatory medications that doctors prescribe for a wide range of illnesses and conditions. We also call them glucocorticoids. They can either be synthetic versions of human hormones. For example, cortisone, a steroid, is a synthetic version of a hormone that the adrenal glands produce. The adrenal glands sit on top of the kidneys. Synthetic means artificial, i.e., not natural.
Synthetic cortisone is extremely effective for lupus patients who experience inflammation, tenderness and pain. However, like some other lupus medications, it can also cause several adverse events, i.e., undesirable side effects. Therefore, doctors only prescribe it when nothing else works.
Regarding steroids, the Johns Hopkins Lupus Center writes:
“The word “steroid” often sounds frightening because of the media attention given to the anabolic steroids that some athletes use to put on muscle.”
“However, it is important to remember that steroids make up a large group of molecules with different functions, and the steroids given to treat lupus – specifically, corticosteroids – are different than those you may hear about on the news.”
The most common undesirable side effects are acne, skin that bruises easily, stunted growth in children, insomnia, and depression. Fluid retention, redistribution of fat, hair growth, and weight gain are also possible side effects.
Antimalarials
Antimalarials are medications that scientists originally designed to cure or prevent malaria. However, doctors subsequently found that they helped control lupus symptoms. Specifically skin rashes and joint pain. Lupus patients with mouth ulcers also benefit from antimalarials.
Doctors sometimes prescribe antimalarials for patients with mild inflammation and blood clotting problems.
Some side effects such as skin color changes and mild tummy upset are possible but extremely rare.
In the Lupus Society of Illinois website, Dr. Robert Katz writes:
“Immunosuppressive drugs may help preserve kidney function, lessen the severity of symptoms and sometimes even put the disease into remission. These drugs also help reduce damage to vital organs.”
Anticoagulants
Some lupus patients have a higher-than-average risk of developing blood clots. Blood clots are life-threatening. Therefore, doctors may prescribe anticoagulants.
Anticoagulants thin the blood. In other words, they prevent the blood from clotting easily. Low-dose aspirin, for example, is an OTC anticoagulant medication. OTC stands for over-the-counter, i.e., you don’t need a doctor’s prescription to buy it.
Heparin and warfarin are examples of prescription anticoagulants.
For some lupus patients, anticoagulants are among the lupus medications that they must take for the rest of their lives.
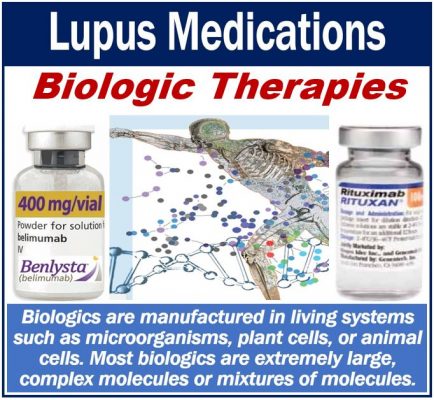
Biologics
We call medications that come from biological rather than chemical sources biologics. Scientists extract them from biological sources. Sometimes, they may also synthesize them.
A biologic medication may consist of nucleic acids, proteins, tissues, or living cells. Some biologics consist of complex combinations of all at least two of these substances.
Belimumab and Rituximab, for example, are biologics that also serve as lupus medications. These medications reduce or remove the activity of B-cells.
B-cells are white blood cells that produce autoantibodies. Autoantibodies are harmful because they attack good cells and tissues.
Arthritis Research UK says the following regarding biologics and carrying an alert card:
“If you’re being prescribed a biological therapy, such as rituximab, it’s recommended that you carry a biological therapy alert card, which you can obtain from your doctor or rheumatology nurse specialist.”
“Then if you become unwell, anyone treating you will know that you’re on a biological therapy and that you’re therefore at risk of its side-effects, including injections.”
Repository Corticotropin Injection
Repository Corticotropin Injection contains Acthar, a natural-occurring purified hormone called ACTH. ACTH stands for adrenocorticotropic hormone.
Researchers believe that Acthar helps the human body produce its own cortisol. It might help the body also produce other steroids.
Cortisol, for example, helps the immune system reduce or prevent inflammation.
In an article published in Lupus Science & Medicine, researchers came to the following conclusion after carrying out a clinical trial:
“RCI demonstrated durable effectiveness in patients with persistently active SLE despite moderate-dose corticosteroid therapy. Switching from placebo resulted in reduced disease activity during the OLE. These data provide the foundation for evaluation of RCI in a robustly powered study.”
SLE stands for systemic lupus erythematosus. RCI stands for repository corticotropin injection.