Lupus treatment options and self-help measures
Although it is currently incurable, there are many lupus treatment options. In most cases, it is very treatable, and patients respond well to certain medications and self-help measures. Lupus treatment is especially effective if it can begin during the early stages of the disease.
Lupus treatment options can ease the symptoms. They can also make it easier for the patient to live with the disease.
This article forms part of the Lupus Collection of articles. It includes: 1. What is lupus? 2. Lupus signs and symptoms. 3. Lupus diagnosis and tests. 4. Causes of lupus. 5. What lupus medications do doctors prescribe?
Treatment options vary considerably
Lupus has many different possible signs and symptoms, which means that no two cases are ever the same. Therefore, lupus treatment options vary significantly, depending on the patient’s signs and symptoms.
Treatment also depends on the severity of the signs symptoms.
In most cases, doctors tend to prescribe many different drugs. That is why the global lupus drugs market is so large.
Flare-ups
A patient’s lupus treatment regime can change, depending on whether they are in the flare-up stage or in between.
Lupus symptoms periodically get worse, then subside, and later on get worse again. In other words, the signs and symptoms go through cycles.
We refer to the more severe period as a ‘flare‘ or ‘flare-up.’
According to the NHS in Scotland, treatment typically involves a combination of medication and self-care measures. NHS stands for the National Health Service.
Lupus treatment options
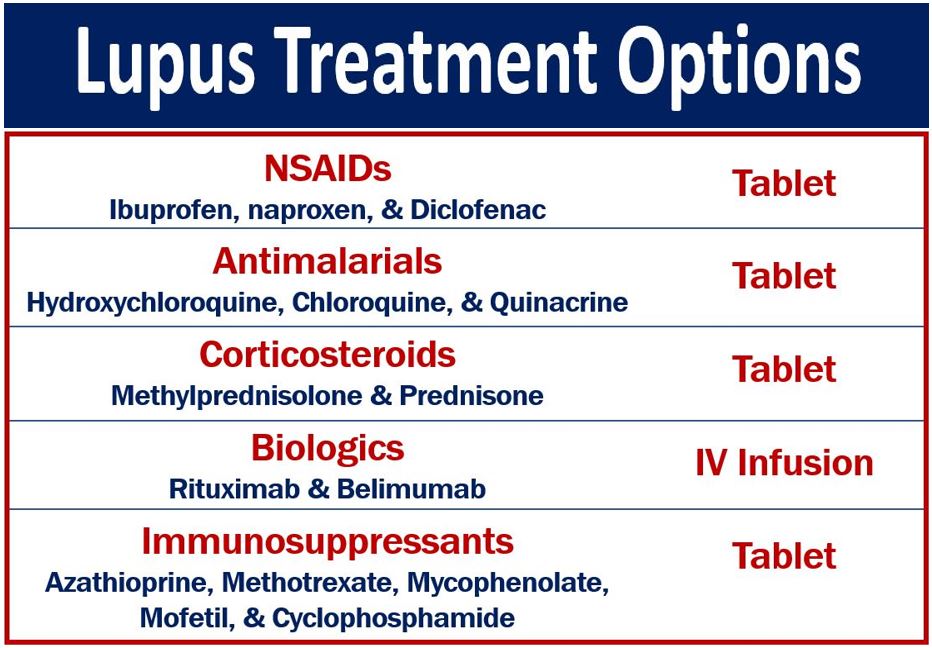
NSAIDs
The letters NSAIDs stand for non-steroidal anti-inflammatory drugs. These are common, OTC, pain-killing medications that reduce inflammation in the human body. OTC stands for over-the-counter, i.e., you can buy OTC drugs without a doctor’s prescription.
An NSAID is a useful lupus treatment option for patients with joint or muscle pain. Ibuprofen and naproxen, for example, are NSAIDs. Diclofenac is also an NSAID.
If the pain is severe, the doctor can prescribe a stronger drug.
NSAIDs not ideal for some patients
Patients with liver, kidney, or stomach problems should not take NSAIDs. If you currently have or had such problems, you need to tell your doctor.
In some cases, people with asthma should not take NSAIDs. Regarding muscle and joint aches and pains, your doctor needs to determine what your best lupus treatment option is.
Regarding NSAIDs for patients with lupus, a PubMed article states the following:
“Up to 80% of patients with systemic lupus erythematosus (SLE) are treated with non-steroidal anti-inflammatory drugs (NSAID) for musculoskeletal symptoms, serositis, and headache.”
Antimalarial drugs for lupus treatment
Antimalarial drugs were initially created to treat or prevent malaria. However, during the Second World War, doctors found that some of them were effective as a lupus treatment.
Subsequently, doctors started prescribing them for patients with lupus.
Hydroxychloroquine, chloroquine, and quinacrine
Hydroxychloroquine (Plaquenil) and chloroquine (Aralen), for example, are antimalarial drugs that doctors often prescribe for patients with lupus. They also prescribe quinacrine (Atabrine).
As a lupus treatment, antimalarials help reduce muscle/joint pain and skin rashes. They also help treat pericarditis and pleuritis. Pericarditis is inflammation of the lining of the heart, while pleuritis is inflammation of the lining of the lung.
Antimalarials also help treat fever and fatigue. Experts say that these medications can help prevent lupus from spreading to the kidneys and the central nervous system.
Antimalarials can help reduce the severity of flare-ups by as much as fifty percent.
Regarding using an antimalarial drug as a lupus treatment, the Johns Hopkins Lupus Center says:
“Plaquenil and other anti-malarials are the key to controlling lupus long term, and some lupus patients may be on Plaquenil for the rest of their lives.”
“For this reason, you can think of anti-malarials as a sort of ‘lupus life insurance.'”
DMARDs
Antimalarials are DMARDs. The letters DMARDs stand for disease-modifying antirheumatic drugs. Doctors prescribe DMARDs in lupus treatment to reduce the incidence of flares.
They also help slow down the progress of the disease and reduce the need for steroid use.
During a flare-up, doctors prescribe DMARDs alongside corticosteroids.
Corticosteroids
Corticosteroids are any group of steroid hormones that we either make synthetically or that the adrenal cortex produces. They have several metabolic functions. Doctors also prescribe them to treat inflammation.
Prednisone
As a lupus treatment, patients take corticosteroids to treat inflammation. Prednisone, for example, is a synthetic corticosteroid that doctors prescribe to suppress the immune system.
In other words, prednisone reduces inflammation by suppressing the immune system.
Methylprednisolone
Doctors may prescribe methylprednisolone for patients with serious disease that involves the brain and kidneys. Medrol and A-Methapred, for example, are methylprednisolone brand names.
Regarding corticosteroid side effect, the Mayo Clinic says:
“Side effects include weight gain, easy bruising, thinning bones (osteoporosis), high blood pressure, diabetes and increased risk of infection.”
“The risk of side effects increases with higher doses and longer term therapy.”
Wikipedia says that methylprednisolone may also trigger mental health problems in some patients.
Immunosuppressants
Immunosuppressants prevent or inhibit immune system activity. As lupus is an autoimmune disease, calming down the immune system makes sense because it reduces the severity of symptoms. We also call them immunosuppressive drugs.
Immunosuppressants work by reducing the number of antibodies in our bloodstream.
A doctor will typically prescribe an immunosupressant as part of a lupus treatment for patients whose symptoms are severe.
Azathioprine, methotrexate, and mycophenolate, for example, are immunosuppressants. Mofetil and cyclophosphamide are also immunosuppressants.
The Lupus Society of Illinois says:
“Immunosuppressive drugs may help preserve kidney function, lessen the severity of symptoms and sometimes even put the disease into remission. These drugs also help reduce damage to vital organs.”
Biologics
Biologics are medications that come from biological rather than chemical sources. We extract them from biological sources or semisynthesize them.
Biologics may consist of living cells, tissues, proteins, or nucleic acids. They may also comprise complex combinations of these substances.
Rituximab and belimumab
Rituximab and belimumab, for example, are biologics that doctors prescribe for lupus treatment. They remove or reduce the activity of B-cells.
A B-cell is a type of white blood cell that produces autoantibodies; these are harmful.
If DMARDs are not effective, doctors may prescribe rituximab or belimumab.
Alert card
Patients on biologics should carry a biological therapy alert card, says Arthritis Research UK.
Arthritis Research UK writes:
“If you’re being prescribed a biological therapy, such as rituximab, it’s recommended that you carry a biological therapy alert card, which you can obtain from your doctor or rheumatology nurse specialist.”
“Then if you become unwell, anyone treating you will know that you’re on a biological therapy and that you’re therefore at risk of its side-effects, including injections.”
Lupus self-help options
There are many self-help measures that patients can take which reduce the severity and frequency of symptoms.
Limiting sunlight exposure
Some lupus patients’ cannot tolerate too much exposure to sunlight. After exposure to sunlight, their risk of skin rashes increases significantly.
Also, if you already have a skin rash, sunlight exposure can make it even worse.
Tropics and summer months
Therefore, it is important for you to limit your skin’s exposure to sunlight. This is especially the case in the tropics or during the summer months.
The best way to protect your skin is to remain indoors or stay in the shade. However, if you have to be in direct sunlight, wear a wide-brimmed hat and sunglasses.
You should also wear clothes that cover as much of your skin as possible.
Sunscreen SPF
Sunscreens with a high SPF also help. SPF stands for sun protection factor. The sunscreen’s SPF compares how long it takes skin with sunscreen to burn versus skin without sunscreen.
For example, an SPF of 2 means it will take twice as long, while an SPF of 10 means ten times as long.
In other words, the higher the sunscreen’s SPF, the more protection the skin gets. Among patients’ lupus treatment options, a sunscreen during the summer months ‘is a must.’
Regarding photosensitivity, the Lupus Foundation of America says:
“Beyond skin rashes that can develop, exposure to the sun can cause those living with lupus to experience increased disease activity with symptoms such as joint pains, weakness, fatigue and fever.”
“Two-thirds of people with lupus have increased sensitivity to ultraviolet rays, either from sunlight or from artificial inside light, such as fluorescent light – or both.”
Regular checkups
Rather than just seeing your doctor when your symptoms get worse, you should undergo regular checkups.
Regular checkups help prevent or reduce the severity of flare-ups.
Regularly seeing a healthcare professional also helps address several health concerns such as diet, stress, and exercise.
Good diet, sleep, and exercise are important for preventing potential lupus complications.
Smoking
Smoking raises the risk of developing cardiovascular disease. It can also exacerbate the effects of lupus on blood vessels and the heart.
If you are a smoker, you should seriously consider giving up.
If the thought of giving up cold turkey puts you off, talk to your doctor about it.
Electronic cigarettes
Electronic cigarettes or e-cigarettes are much less harmful than tobacco smoking.
If you are heavily addicted to nicotine, try switching to e-cigarettes. However, giving up completely is the best lupus treatment option.
You might find it easier to wean off e-cigarettes than tobacco cigarettes.
Vitamin D
Kaleidoscope Fighting Lupus quotes studies which suggest that 67% of lupus patients are vitamin D deficient.
We also know that lupus patients with high vitamin D levels have fewer symptoms than their deficient counterparts. Additionally, their symptoms are less severe.
Cardiovascular problems
People with lupus who have low vitamin D levels have a higher risk of developing heart disease. Also, vitamin D deficient lupus patients are more likely to suffer from hypertension and elevated lipid levels. Hypertension means high blood pressure.
Flare-ups
Some studies suggest that taking vitamin D supplements can reduce a lupus patient’s chances and occurrences of flare-ups.
Regarding vitamin D levels and lupus, Kaleidoscope Fighting Lupus says:
“While the research is certainly interesting and even promising, there is no conclusive research that shows that low vitamin D levels cause lupus nor can the physiological and clinical significance be confirmed.”
“It is also difficult for researchers to determine whether low levels of vitamin D cause lupus or whether the lupus causes the low levels of vitamin D.”
Vitamin D research
Ask your doctor whether he or she believes that your lupus treatment should include vitamin D supplements. There is a lot of research taking place at the moment.
Complementary and alternative medicines
Alternative medicine does not have the same meaning as complementary medicine.
Complementary medicine
Complementary medicine exists alongside conventional medicine. In other words, if you receive complementary medicine, you also receive conventional medicine.
Alternative medicine
Alternative medicine replaces conventional medicine. In other words, if you are receiving alternative medicine, you don’t receive conventional medicine.
Examples of these diverse medicines, i.e., either alternative or complementary medicines, include massage therapy, acupuncture, biofeedback, and herbs. Ayurveda, naturopathy, and homeopathy are other examples.
Scientific testing and clinical research
Conventional medicine is based on rigorous scientific testing. Complementary and alternative medicine have not been through the same level of scientific testing and clinical research.
Therefore, regarding lupus treatment, it is difficult to know how effective they are.
This quote, regarding herbal supplements, comes from the Lupus Foundation of America:
“In fact, some herbal supplements can make a person’s lupus symptoms worse, or interact in a harmful way with the medicines a doctor has prescribed.”
“Therefore, before beginning any complementary or alternative therapy, it is very important for people with lupus to discuss these practices with their doctor (especially if planning to use herbs or supplements).”
Acupuncture, biofeedback, and meditation
The Lupus Foundation of America adds that some studies have shown that acupuncture helps with arthritis pain. Meditation and biofeedback techniques may also help with pain management.
Lupus UK has an interesting web page titled ‘Alternative and Complementary Medicine in the Treatment of Lupus.’
Video – Lupus treatment
In this Johns Hopkins Rheumatology video, Dr. George Stojan talks about various lupus treatment options. The goal of treating lupus, he says, is always remission.
Dr. Stojan is Assistant Professor of Medicine at the Johns Hopkins Lupus Center.

