Lupus is a chronic, i.e., long-term condition that causes inflammation of the joints and other organs. It also causes inflammation of the skin. Doctors do not know what causes lupus. However, patients’ symptoms can improve considerably if they get an early diagnosis and prompt treatment. The medical term for the disease is Systemic Lupus Erythematosus (SLE).
A systemic disease is one that affects either the body as a whole or several organs and tissues. The word ‘systemic’ means ‘related to a system’ rather than to a particular part.
Doctors often misdiagnose patients with lupus. It’s signs and symptoms are often similar to those of other conditions and diseases.
Although nobody is certain what causes lupus, experts believe there are certain triggers. They say that certain medications, infections, and even sunlight may trigger the disease.
The Mayo Clinic in the United States has the following definition of the SLE:
“Lupus is a systemic autoimmune disease that occurs when your body’s immune system attacks your own tissues and organs. Inflammation caused by lupus can affect many different body systems.”
In 14th-century Britain, people started using the term for diseases that caused skin ulcerations. It came from the Medieval Latin word Lupus, which meant ‘wolf.’ According to etymonline.com, people adopted the word because the disease ‘devours’ the affected part.
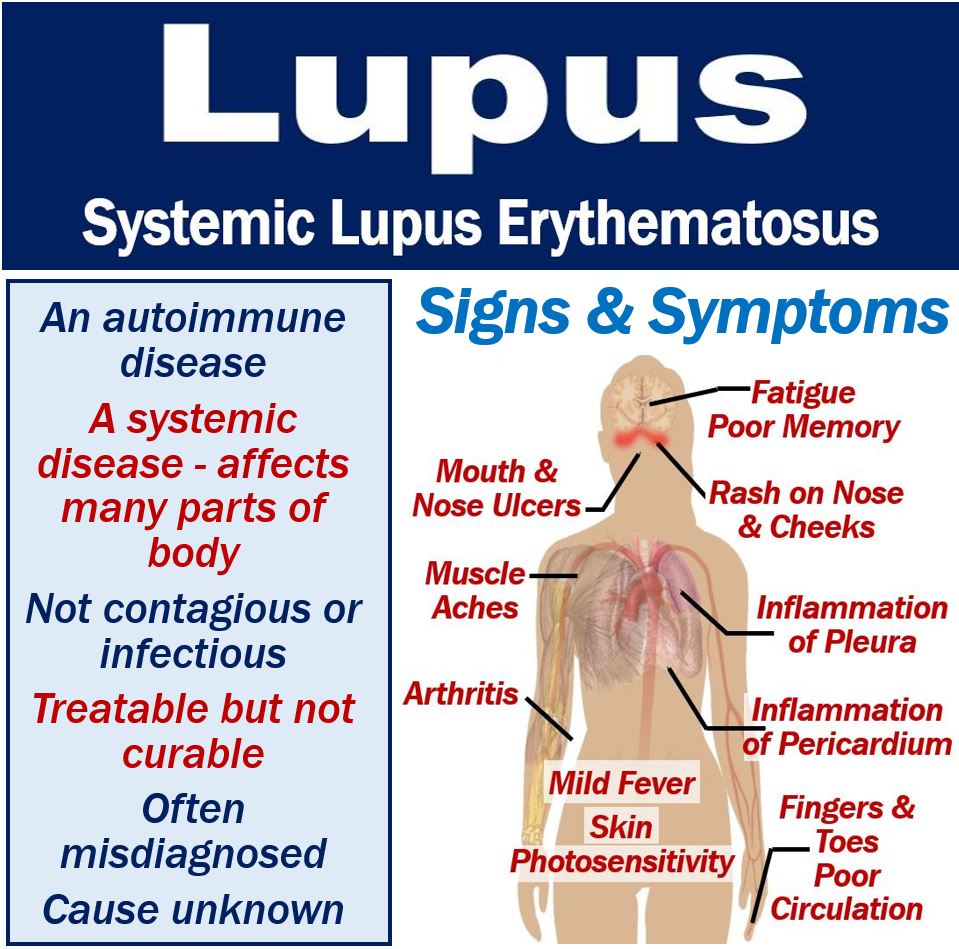
Lupus – signs and symptoms
A symptom is something the patient experiences and describes, such as a headache. Nobody else can detect it. A sign, on the other hand, is something other people may detect, such as a rash.
Medical experts refer to lupus as ‘the great imitator.’ This is because it frequently mimics the signs and symptoms of other diseases and conditions.
Therefore, diagnosis is often elusive. In fact, some patients may suffer for years before getting an accurate diagnosis.
At MBN Health, we have another article that looks at the signs and symptoms of SLE in more depth.
Most common signs and symptoms
The full name of the disease, “lupus erythematosus,” translates to “red wolf” in Latin, which is thought to relate to the red, wolf-bite-like lesions that appear on the skin of those affected.
According to the UK’s National Health Service, following signs and symptoms are also common:
– Stiffness and joint pain.
– Fatigue, i.e., extreme tiredness. Even after plenty of rest, the patient still feels exhausted.
– Rashes, usually over the cheeks and nose.
Other possible signs and symptoms are:
- Swollen glands.
- Photosensitivity, i.e., sensitivity to light. Exposure to sunlight can cause skin rashes.
- Raynaud’s phenomenon. Due to poor circulation to fingers and toes, they can turn blue or white when exposed to cold. Stress may also have the same effect.
- Elevated body temperature, i.e., fever.
- Headaches.
- Memory loss and confusion.
- Chest pain.
- Dry eyes.
- Some patients may experience shortness of breath.
If you frequently have joint pain, stiffness, extreme fatigue, and skin rashes, you should see a doctor.
Signs and symptoms may develop gradually or appear suddenly. Some patients have mild symptoms while for others they are severe.
They may last for a long time, and could even be permanent. In other cases, the signs and symptoms are temporary.
Flare-ups
In the majority of cases, patients have flare-ups. Flare-ups, in this context, refers to episodes when signs and symptoms become more severe.
However, they subsequently get better and sometimes disappear altogether. Then, after a while, they come back, i.e., the next flare-up begins.
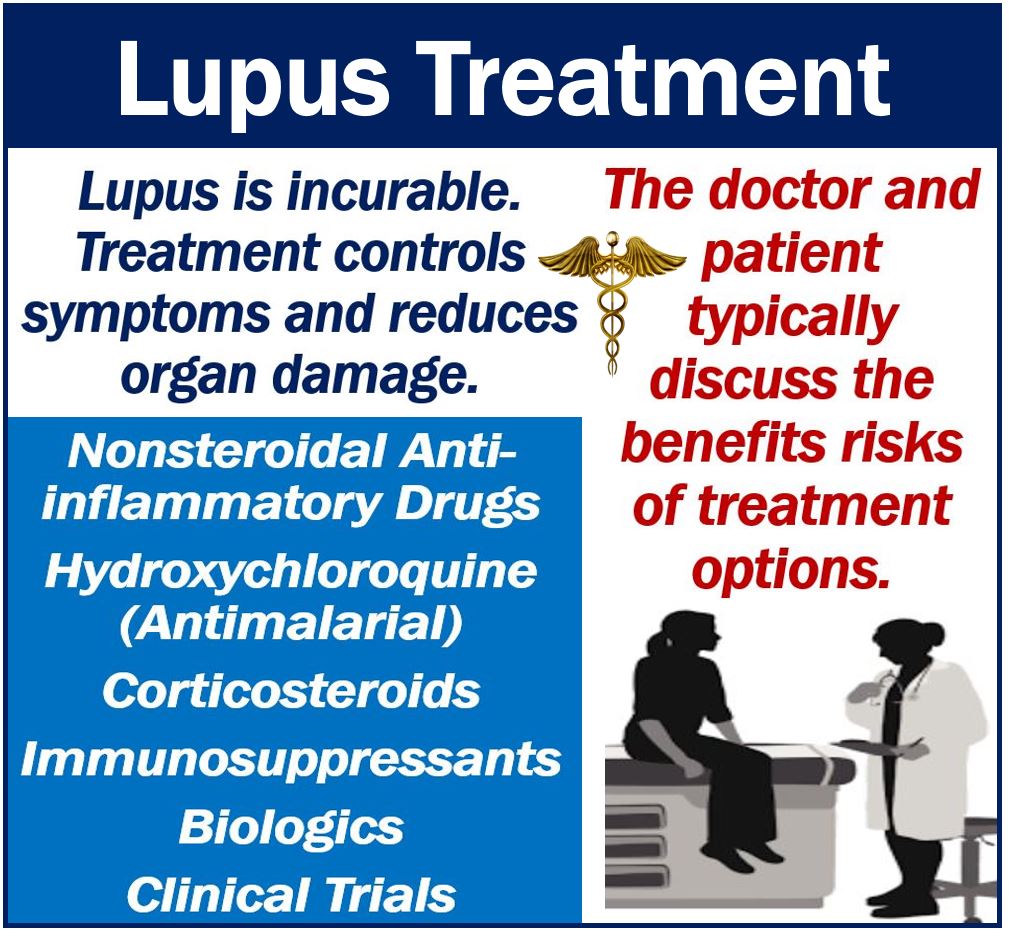
Lupus – treatment
Patients’ treatments depend on what parts of the body are affected and how severely. In other words, what your doctor prescribes depends on your signs and symptoms.
Lupus is incurable. Treatments can only reduce the severity of symptoms and protect organs.
Determining what a patient’s best treatment is can be tricky. Often, the doctor and patient discuss options, try them out, and pursue the ones that work best.
Symptoms flare-up and then subside. As the severity of signs and symptoms change, medications and dosages also change.
At MBN, we gave in-depth article on lupus treatment options and self-help suggestions as well as one on the medications that doctors prescribe.
Most common medications
Below is a list of the most common medicines that doctors prescribe.
- Steroid creams, tablets, and injections for rashes and kidney inflammation.
- Anti-inflammatory medication such as ibuprofen.
- For joint problems and fatigue, the doctor may prescribe hydroxychloroquine. This drug is an antimalarial.
- Most of these medications were initially developed for other diseases. However, doctors later found that they also helped lupus patients.
- Immunosuppressants. These drugs prevent or inhibit activity of the immune system. Lupus is an autoimmune disease, so calming down the immune system makes sense. Immunosuppressants reduce the number of antibodies in the bloodstream. Doctors generally prescribe immunosuppressants for patients with severe lupus.
- Biologics. Biologics are manufactured in living systems such as animal cells, plants, or microorganisms. They are either extremely complex molecules or mixtures of molecules. Rituximab and belimumab, for example, reduce the activity of B-cells. These are white blood cells that produce harmful autoantibodies.
If you are undergoing biological therapy, you should carry a biological therapy card. Healthcare professionals need to be aware of this when they treat you.
Arthritis Research UK offers patients the following advice:
“If you’re being prescribed a biological therapy, such as rituximab, it’s recommended that you carry a biological therapy alert card, which you can obtain from your doctor or rheumatology nurse specialist.”
“Then if you become unwell, anyone treating you will know that you’re on a biological therapy and that you’re therefore at risk of its side-effects, including injections.”
Lupus – causes
Medical specialists and researchers do not fully understand what causes lupus. The following may trigger the condition:
- Medications.
- Giving birth, i.e., childbirth.
- The menopause.
- Sunlight exposure.
- Puberty.
- Infections. Particularly viral infections.
In the United States, health authorities say that Lupus is more common among Asian-Americans, African-Americans, and Hispanics. In the USA, ‘Hispanics’ refers to Latin Americans, i.e., not Spaniards.
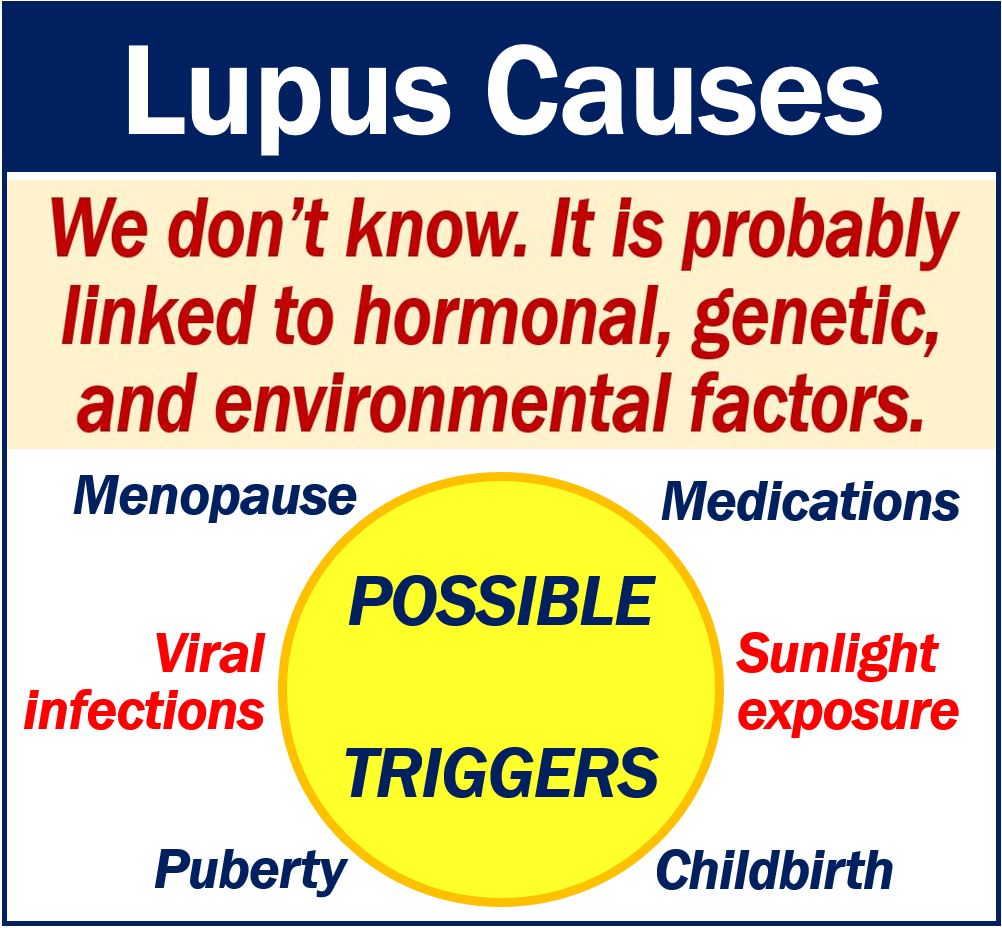
The National Resource Center on Lupus in the USA says that many scientists, but not all, believe that lupus is the result of a combination of factors.
These factors include genetics, hormones, and the environment. In other words, factors inside and outside the human body.
LUPUS UK emphasizes that Lupus is neither infectious nor contagious.
Lupus – life expectancy
Between 80% and 90% of patients have normal life spans says Lupus.org. Specifically, patients with close follow-up and treatment.
For the vast majority of sufferers, it is not fatal, i.e., they will not die from it.
The condition may be life-threatening for patients who have severe flare-ups.
Pharmaceutical companies predict that the lupus drugs market will grow significantly over the next ten years.
Video – What is Lupus
This educational video, from our sister channel on YouTube – Marketing Business Network, explains what ‘Lupus’ is using simple and easy-to-understand language and examples.